Despite the importance of health care fraud and the political, legislative and administrative attentions paid to it, combating fraud remains a challenge to the health systems.
We aimed to identify, categorize and assess the effectiveness of the interventions to combat health care fraud and abuse.
Methods
The interventions to combat health care fraud can be categorized as the interventions for ‘prevention’ and ‘detection’ of fraud, and ‘response’ to fraud. We conducted sensitive search strategies on Embase, CINAHL, and PsycINFO from 1975 to 2008, and Medline from 1975–2010, and on relevant professional and organizational websites. Articles assessing the effectiveness of any intervention to combat health care fraud were eligible for inclusion in our review. We considered including the interventional studies with or without a concurrent control group. Two authors assessed the studies for inclusion, and appraised the quality of the included studies. As a limited number of studies were found, we analyzed the data using narrative synthesis.
Findings
The searches retrieved 2229 titles, of which 221 full-text studies were assessed. We found no studies using an RCT design. Only four original articles (from the US and Taiwan) were included: two studies within the detection category, one in the response category, one under the detection and response categories, and no studies under the prevention category. The findings suggest that data-mining may improve fraud detection, and legal interventions as well as investment in anti-fraud activities may reduce fraud.
Discussion
Our analysis shows a lack of evidence of effect of the interventions to combat health care fraud. Further studies using robust research methodologies are required in all aspects of dealing with health care fraud and abuse, assessing the effectiveness and cost-effectiveness of methods to prevent, detect, and respond to fraud in health care.
Introduction
Fraud has been defined as an “intentional deception or misrepresentation made by a person or an entity, with the knowledge that the deception could result in some kinds of unauthorized benefits to that person or entity” [1]. Because of complexities of defining fraudulent behavior and detecting fraudulent cases, measuring fraud losses in health care is difficult [2]. Undetected frauds remain a problem; in many individual cases, it may not be possible to determine whether a claim is fraudulent or not. Still, it has been estimated that three to ten per cent of health care spending is lost to health care fraud and abuse, amounting to billions of dollars per year [3],[4].
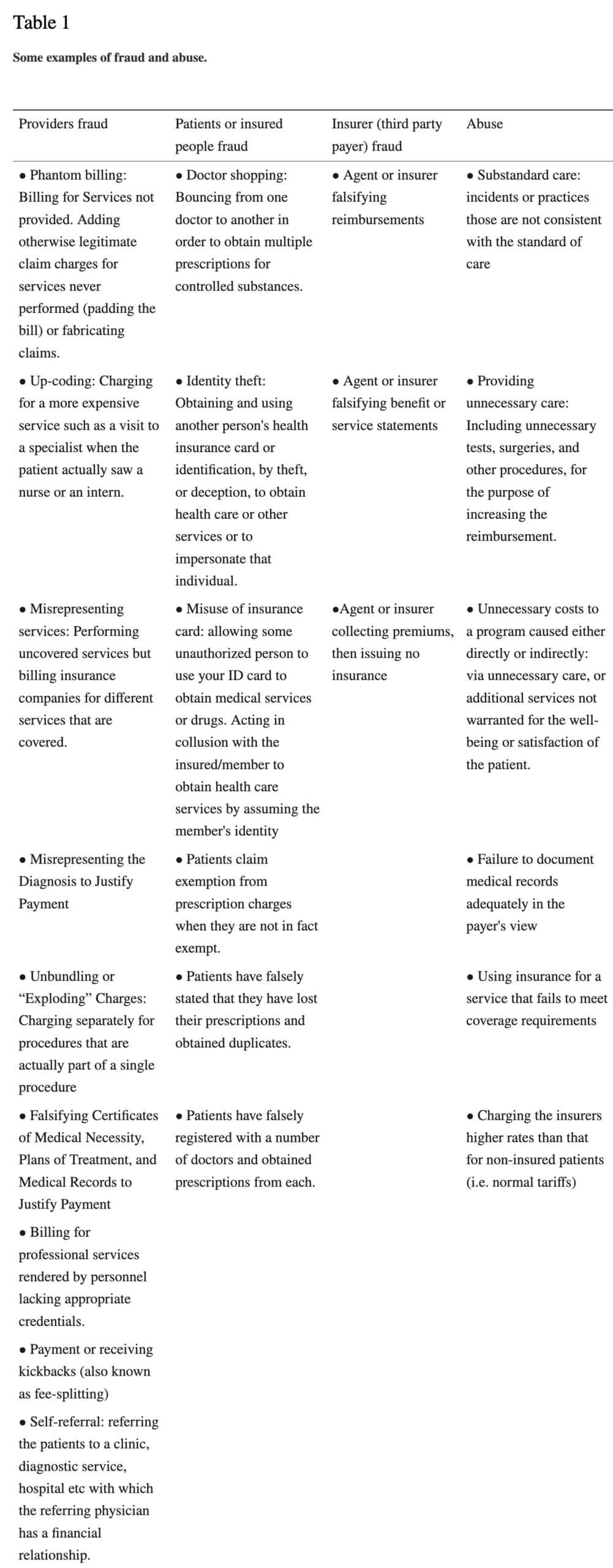
In general, fraud incorporates the following elements: misrepresentation of a material fact, knowledge of the falsity of the misrepresentation, intent, a victim that can be a person or organization acting on the misrepresentation, and damage to the victim [5]. Fraud boundaries are confused with other concepts such as error, negligence, abuse, and corruption. Abuse is the closest concept to fraud and usually accompanies it. The degree of intent by the individual or entity is often the determining factor in distinguishing between fraud and abuse. The term “abuse” may be used to describe problematic behavior which is not clearly against the law or where certain elements of the fraud definition (such as knowing deception) are missing [6].
Despite the importance of fraud and the varying levels of political, legislative, and administrative attention paid to it, combating health care fraud remains an important challenge to the health systems. Sparrow (1998), in his review of public sector fraud, suggested that several factors explain why combating fraud is difficult: the amount of fraud identified by the detection systems is never the real scale of the problem; the fraud control performance indicators are ambiguous and misleading; the amount of resources available to combat fraud remains limited; combating fraud is a dynamic process and requires continuous change; and too much reliance is placed on traditional enforcement approaches (such as case-note reviews which are costly to conduct and lack reliability) [2].
Health care systems are particularly vulnerable to fraud and corruption [7]. Many factors including the asymmetry of information between providers and patients, inelastic demand for services, the enormous volume of money spent on health care, the presence of third-party and fee-for-service payments, and the public trust in providers, exacerbate the problem within the health care sector [8],[9].
Classification and typology of health care fraud
Based on who conducts the fraud, we can classify fraud into categories of provider fraud, consumer fraud (patient or insured), and insurer or payer fraud [10]. Provider health care fraud may be committed by individuals (e.g. physicians, dentists) or by provider organizations (e.g. hospitals). Sometimes providers engage in frauds that involve other service providers (e.g. diagnostic services) or pharmaceutical and medical device manufacturers by receiving kickback payments (See Table 1).
Arash Rashidian, Hossein Joudaki and Taryn Vian – National Library of Medicine – 2012-08-24.